Cardiomyopathy in Children: Awareness, Prevention and Care Options

Though adults are usually the focus when we talk about heart disease, children can also face serious heart conditions. Childhood heart problems are rare, and congenital heart defects (CHD) often come to mind first. But cardiomyopathy is another serious condition that affects children.
Cardiomyopathy impacts the heart muscle, making it harder for the heart to pump blood properly. While it may not be as commonly discussed as CHD, it can have serious consequences for growth, development, and overall well-being. The challenge is that many families do not realize that young children may also face such conditions, which means diagnosis is often delayed.
By spreading awareness, offering clear information, and supporting parents with the right resources, we can help ensure children with cardiomyopathy receive care at the earliest stage possible. Early conversations about this condition open the door to better health outcomes and stronger support systems for families.
What is Cardiomyopathy in Children?
Cardiomyopathy is a disease of the heart muscle that reduces its ability to pump blood efficiently. Over time, this weakness or stiffness in the heart muscle can lead to heart failure, life-threatening arrhythmias, or even sudden cardiac arrest.
Unlike adult heart disease, which is often linked to lifestyle factors like smoking, obesity, or diabetes, cardiomyopathy in children is more often associated with genetic factors, infections, or underlying medical conditions.
Why Awareness of Cardiomyopathies is So Important?
Unlike congenital heart defects (CHD), which are often detected soon after birth, cardiomyopathy can develop months or even years later. This makes it trickier to spot, and many children don’t show obvious symptoms until the condition has progressed.
Reasons awareness is important:
- Silent progression: A child may appear healthy but still have underlying heart muscle weakness.
- Misdiagnosis risk: Fatigue, poor appetite, or fainting might be mistaken for minor health issues or even “laziness.
- High-risk outcomes: Cardiomyopathy is a leading cause of sudden cardiac death in young athletes. Many tragic incidents reported globally, including in India, involve children collapsing during school sports.
- Better prognosis with early care: When diagnosed early, many children can manage the disease with medication and lifestyle changes, avoiding severe complications.
Imagine a 10-year-old boy in a school football match. He faints suddenly on the field. While everyone assumes it’s dehydration, later evaluation reveals hypertrophic cardiomyopathy (HCM) — a condition that thickens the heart muscle. If caught earlier, this risk could have been managed with monitoring and activity restrictions.
This is the reason awareness campaigns are essential not just among parents, but also teachers, coaches, and healthcare providers.
Types of Cardiomyopathy Conditions in Children
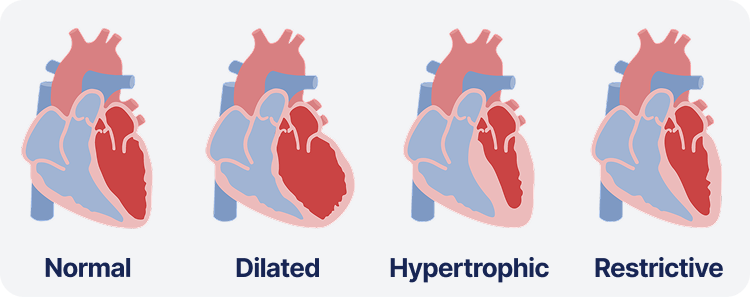
There are three main types of cardiomyopathy conditions seen in children. Knowing each of them well is better as it requires a different approach to care.
1. Dilated Cardiomyopathy (DCM)
This is the most common type found in children. In dilated cardiomyopathy, the heart muscle becomes weak and stretched, which reduces the ability of the heart to pump blood efficiently. Children with DCM may appear unusually tired, may struggle with feeding, or may have trouble gaining weight. In severe cases, it can lead to heart failure.
2. Hypertrophic Cardiomyopathy (HCM)
In hypertrophic cardiomyopathy, the heart muscle becomes abnormally thick. While it may not always cause symptoms, it can make it harder for the heart to relax and fill with blood. This condition is sometimes linked with sudden cardiac arrest in young athletes, making it particularly concerning.
3. Restrictive Cardiomyopathy (RCM)
This is one of the rarest types in children. In restrictive cardiomyopathy, the heart muscle becomes stiff, making it difficult for the heart to fill properly with blood. As a result, the heart cannot supply the body with enough oxygen, which can cause fatigue, swelling, and difficulty breathing.
4. Other Rare Types of Cardiomyopathy in Children
There are other forms like arrhythmogenic right ventricular cardiomyopathy and left ventricular non-compaction. Although rare, they can still pose serious risks and require specialized medical attention.
Causes of Cardiomyopathy in Children
The causes vary widely and can be as follows:
- Genetic mutations (inherited conditions)
- Infections (viral myocarditis damaging the heart muscle)
- Metabolic or mitochondrial disorders
- Autoimmune diseases
- Toxin or chemotherapy exposure
- Unknown causes (idiopathic) – nearly half of cases, no clear reason found
Symptoms of Cardiomyopathy Every Parent Should Look For
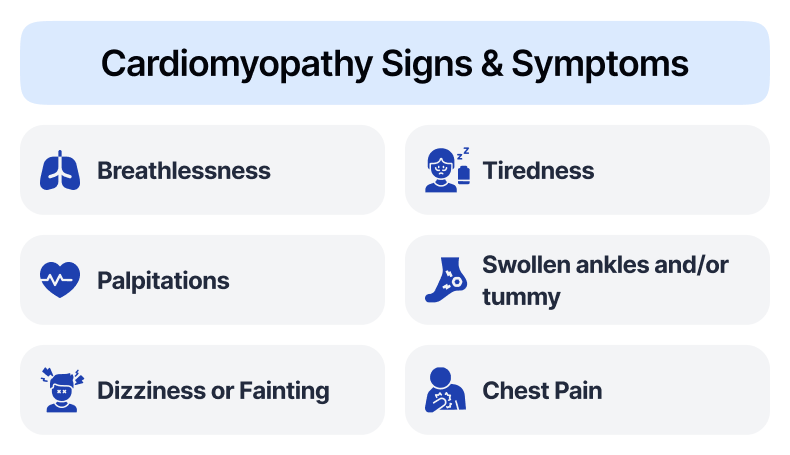
The tricky part is that symptoms often mimic common childhood issues. Parents should be alert if their child shows:
- Fatigue or low energy
- Shortness of breath (especially during play or at night)
- Swelling in the legs, ankles, or abdomen
- Fainting spells or dizziness
- Rapid or irregular heartbeat
- Difficulty feeding (in infants)
- Poor growth or weight gain
These may or may not always mean heart disease, but if they persist or worsen, a pediatric cardiology evaluation is necessary.
Diagnosis: How Doctors Detect Cardiomyopathy in Children?
Diagnosing cardiomyopathy requires a combination of medical history, physical examination, and advanced tests.
Doctors may use echocardiograms, electrocardiograms (ECG), chest X-rays, or cardiac MRI to look closely at the heart’s structure and function. Genetic testing may also be recommended, especially if there is a family history of the condition.
Early diagnosis makes a difference. Children who are diagnosed in the early stages can often be managed with medications and lifestyle changes before the condition progresses to more severe outcomes.
Treatment Options Available for Cardiomyopathic Conditions in Children
Treatment depends on type and severity, but it usually involves a mix of:
Medications
Drugs may be prescribed to manage symptoms, improve heart function, or regulate heart rhythm. These include beta-blockers, ACE inhibitors, and diuretics.
Lifestyle Management
Adjustments in daily activities may be recommended, such as limiting strenuous exercise, following a healthy diet, and monitoring fluid intake.
Medical Devices
In severe cases, devices like pacemakers or implantable cardioverter defibrillators (ICDs) may be used to regulate heart rhythm and prevent sudden complications.
Surgery and Transplants
For children with advanced cardiomyopathy who do not respond to other treatments, surgery or heart transplantation may be necessary.
Prognosis: Living with Cardiomyopathy and Long-Term Care in Children
The long-term outlook for children with cardiomyopathy depends on the type, severity, and how early it is detected. Some children live relatively normal lives with regular monitoring and medications, while others may face more serious challenges.
Ongoing care is a must. Children with cardiomyopathy need regular check-ups, tests, and sometimes lifelong treatment. Emotional and psychological support for both the child and the family also plays an important role in long-term care.
The Role of AI & Healthtech in Pediatric Heart Care
Technology is reshaping how we detect and manage pediatric heart conditions:
- AI-powered ECG analysis can flag early arrhythmias.
- Wearables (like smartwatches) monitor heart rate and detect abnormalities.
- Remote monitoring apps help doctors track a child’s progress at home.
- Predictive analytics identify children at higher risk of CVD complications.
For rare diseases like cardiomyopathy, AI offers hope for faster diagnosis, personalized treatment, and better long-term outcomes.
Raising Awareness: What Parents Can Do to Support Children with Cardiomyopathy?
According to the Pediatric Cardiomyopathy Registry (PCMR), about 1 in 100,000 children are diagnosed with cardiomyopathy each year worldwide.
- Know the symptoms and seek early evaluation.
- Share family medical history. Many cases are genetic.
- Join support groups to connect with other families.
- Advocate for better healthcare access especially in underserved communities.
- Encourage healthy routines: balanced diet, safe activity, regular check-ups.
Awareness campaigns and conversations reduce stigma and ensure that no child suffers in silence.
Protecting Little Hearts for a Better Future!
Cardiomyopathy in children is rare, but its impact is profound. From genetic inheritance to environmental triggers, it can silently affect young hearts, often without warning.
Helius Wellness strongly believes that with early diagnosis, advanced treatment, and parental awareness, many children can live healthier, fuller lives.
Technology, AI, and community awareness add another layer of hope, ensuring that families don’t feel alone in this fight.
Every child deserves a strong, healthy heart and together, we can make that possible.
Popular Blogs

Agentic AI-Driven Healthcare Revolution
Agentic AI in healthcare for personalised care and real-time decisions.

Artificial Intelligence in Healthcare: A New Approach t...
Chronic disease care with AI wearables, remote monitoring, and more.

AI and Hallucinations in Healthcare Field: A New Fronti...
Know how AI supports the detection and treatment of hallucinations.
